What is a migraine?
Migraine is a complex neurological disorder affecting 1 in 7 people. It is a complex multi-gene disorder affecting brain cell function. 40 migraine genes have been identified, which can be inherited in multiple combinations, making each migraineur unique. The frequency and severity of migraine attacks vary throughout life, and between sufferers. While some suffer one migraine in their life, 4% have chronic daily migraine; that is 8 or more migraines and 15 headache days per month.
What does a migraine feel like?
A migraine attack usually lasts between 4-72 hours. The International Classification of Headache Disorders define migraines in 2 different entities; migraine with aura and without aura. The headache is initially unilateral location, pulsating quality, moderate or severe intensity, aggravation by routine physical activity and association with nausea and/or photophobia (light sensitivity) and phonophobia (sound sensitivity). The aura can cause visual (frosted glass, colourful patterns), sensory (tingling, numbness), motor (weakness) or speech disturbance. By definition, it is a disabling headache disorder.
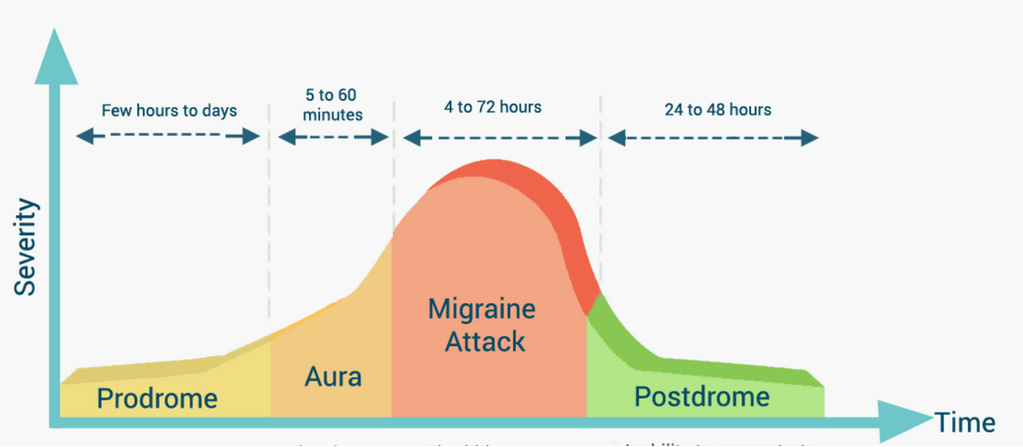
Phases of a migraine
Migraine has multiple phases: premonitory, aura, headache, post-drome and interictal (in between headaches). The premonitory phase can occur 3 days before the headache phase, and it involves complex interactions between various parts of the brain. The headache phase involves activation of the pain system.
The premonitory phase includes food cravings, fatigue, mood changes, yawning, muscle tenderness and photophobia. Various parts of the brain are activated during the premonitory phase. It is important to acknowledge this when one considers the role of food as a “trigger” for migraine headaches, as food cravings could result from the premonitory phase.
(Migraine Buddy, 2015, Blau J N Lancet, 1992)
Does food affect migraine?
There is no conclusive evidence that any particular food causes migraine. The evidence is based on very small numbers of volunteers. All studies which point to a possible link between certain food and migraine attacks are based on dietary diaries. This type of research has large potential for bias. Alcohol, chocolate, caffeine, dairy products such as aged cheese, food preservatives, monosodium glutamate (MSG), and artificial sweeteners have all been studied as migraine triggers.
Caffeine:
Caffeine is found in varying quantity in coffee, tea, chocolate, fizzy drinks and many painkillers. There is plenty of evidence that caffeine with analgesia can abort migraine attacks, and there is evidence that caffeine withdrawal can also cause migraines. Depending on genetic combination, 200-400mg/day of caffeine (a single shot of coffee contains 63mg caffeine; a 50g bar of chocolate between 10-20mg) can benefit mood and reduce depression, although higher doses can cause anxiety. There is evidence in children (3-15 years of age) with reasonable link between caffeine and migraine occurrence, but the same evidence has not been found in adults.
Chocolate:
Chocolate has been self-reported to have caused migraines in 2-22% of people. However, only 2.5% of patients have consistently found any difference by eliminating chocolate from their diet. Factual data on chocolate is very scarce, with the largest study of 81 females suggested no effect. It is important to note that chocolate contains caffeine, milk, sugar and other ingredients, which confound the findings.
Alcohol:
Alcohol is often reported to affect migraines. 40% of patients suggest a link between drinking alcohol and migraines. Wines with histamine content, which include most red wines, are more strongly associated with migraine attacks compared to other alcoholic beverages.
Artificial sweeteners:
Aspartame has been consistently linked with migraines. Small studies giving high doses of aspartame suggested aspartame triggers migraines, although these doses are higher than in standard food portions.
Comprehensive diets:
LOW FAT: 2 small studies suggest low fat diets (<20% of total calories coming from fat) can reduce frequency of migraine attacks. This would equal to roughly 400 calories a day or 45g of fat/day for a 2000 calories diet.
KETO: In contrast, a study of 45 migraine sufferers randomised to a Keto diet (very low carbohydrates and high protein and fat content) showed 75% reduction of migraine attacks in the Keto group compared to normal carbohydrate group. As the Keto group slowly increased the carbohydrate load, their headaches returned. This counters the low fat theory.
What about supplements?
High doses of magnesium (300-500mg/day) and high dose riboflavin (200mg/day) can improve migraine attacks in 30% of sufferers.
A large trial showed omega-3 supplement had no beneficial effect on migraine frequency. There is also no evidence for Feverfew, vitamin D and other vitamins.
A small study showed taking a multispecies probiotic daily over a 10 week period reduced migraine frequency and need for painkillers.
Another small study showed coenzyme Q10 could also reduce the number of migraine attacks.
Summary
Migraine is a complex genetic brain disorder. Dietary links are tenuous, but deserve considering as some people may benefit from changes described above. If you choose to eliminate an item or start a diet for migraine, it must be adhered to for 4-8 week at a minimum. In general, eat natural and avoid artificial food.
REFERENCES:
1. Martin VT and Vij B. Diet and Headache Part 1. Headache 2016. 56(9):1543-52
2. Martin VT and Vij B. Diet and Headache Part 2. Headache 2016. 56(9):1553-62




